|
New
Pre-Denial Process To
Expedite Claims
Expected to decrease administrative delays
by up to 85%
LOUISVILLE, KY--Harmona Healthcare, one of the nation's
largest managed care insurance payors, has announced plans to introduce
"Pre-Denial" of claims to all of its members beginning in the
first quarter of 2001.
 |
|
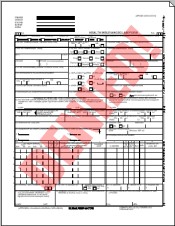
New "Pre-Denied"
Claim Form
|
According to Harmona spokesperson Richard Leikie,
"Pre-Denial" will eliminate 80% of claims processing delays,
and is expected to galvanize sagging profits at the HMO, which also operates
clinics throughout the southeastern U.S. and nationally.
"The way it works is this," said Leike.
"Rather than having a member waste their time filling out a complicated
form and sending it to us, only to find out a month later that we denied
it, what we're going to do is give our members the option of filling out
our new 'Pre-Denial' form, which they'll address and send to themselves
instead."
"That way, they'll find out about their claim
denial in as few as two to three days on average, though it may be slightly
longer during busy mail seasons."
Leike added that members would also be given the
option, for a nominal fee, of using USPS Priority Mail, Express Mail,
or Federal Express Overnight for considerably faster notification of their
claim denial.
 |
|
Harmona Headquarters, Louisville,
KY
|
"Basically, we're putting the control back into
the hands of the consumer," continued Leike. "Survey after survey
tells us the same thing: no one likes to wait weeks or months for their
claim to be processed. Now, if someone says, 'I've gotta know by noon
tomorrow,' they just fill out the form, address an envelope to themselves,
and drop it all off at Fed Ex before 6PM. You better believe they'll have
their answer by morning!"
Reportedly, "Pre-Denial" will be offered
to participating Harmona physicians as early as fall 2001, in order to
accelerate processing of authorization requests for urgent diagnostic
tests and procedures.
|